Simple Foot Exercises That Support Balance and Comfort

Strong, flexible feet are important for overall stability and daily comfort. Simple foot exercises can help improve balance, prevent injury, and ease discomfort caused by tight muscles or weak foot structures. Activities like toe curls, heel raises, and rolling a ball under the arch can strengthen muscles and improve circulation. Stretching the toes and calves can also help relieve tension that may contribute to common foot problems. Practicing balancing on one foot builds stability and can reduce the risk of falls, especially in older adults. Over time, these exercises support better posture and may ease pressure on the ankles, knees, and hips. Making foot exercises part of your routine can help maintain healthy movement and reduce discomfort. If you experience ongoing pain or have difficulty with balance, it is suggested you schedule a visit with a podiatrist for evaluation and guidance.
Exercising your feet regularly with the proper foot wear is a great way to prevent injuries and build strength. If you have any concerns about your feet, contact one of our podiatrists from Pima Foot and Ankle Surgery. Our doctors can provide the care you need to keep you pain-free and on your feet.
Exercise for Your Feet
Exercise for your feet can help you gain strength, mobility and flexibility in your feet. They say that strengthening your feet can be just as rewarding as strengthening another part of the body. Your feet are very important, and we often forget about them in our daily tasks. But it is because of our feet that are we able to get going and do what we need to. For those of us fortunate enough to not have any foot problems, it is an important gesture to take care of them to ensure good health in the long run.
Some foot health exercises can include ankle pumps, tip-toeing, toe rises, lifting off the floor doing reps and sets, and flexing the toes. It is best to speak with Our doctors to determine an appropriate regimen for your needs. Everyone’s needs and bodies are different, and the activities required to maintain strength in the feet vary from individual to individual.
Once you get into a routine of doing regular exercise, you may notice a difference in your feet and how strong they may become.
If you have any questions please feel free to contact our offices located in . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Exercise for Your Feet
Foot and ankle pain can be a nuisance in a person’s life, especially if it happens frequently. The best way to prevent this type of pain, is to exercise often. Regular exercise of the foot includes stretching and strength exercises. Stretching exercises can help prevent injuries such as a sprained ankle, while strength exercises can prevent ailments such as plantar fasciitis.
Stretching exercises can help improve flexibility and the foot and ankle’s range of motion. These exercises can certainly help with those who participate in high-energy activities such as sports. Many athletes routinely perform foot and ankle exercises to prevent injuries like sprained ankles, which are common injuries where the tendons in the ankle are over stretched. Strength exercises help develop foot muscles for better support and protection.
Most exercises are simple and can be done at home, either standing or sitting. One chair exercise is called “limber up”. In this exercise, a person would start by sitting down with their feet flat on the floor. Then lift one leg up so the feet are not touching the floor, then rotate your foot clockwise 15-20 times, and 15-20 times counterclockwise. Repeat the same process with the opposite leg. Another sitting exercise helps stretch the back of your heel and requires an exercise band. It begins by looping the band around a heavy piece of furniture, or something stable that will not be moved when the band is tugged or pulled. Then sit directly in front of it, and slide one foot into the loop, so that the band curves around the forefoot. Start by pulling the forefoot back and holding it for 5-10 seconds. Doing this 10-15 times on each foot, will stretch the back of your heel, increasing your flexibility.
Foot exercises that require standing are also just as easy and simple. Referred as the “Achilles Stretch”, this exercise stretches the Achilles tendon, making it more flexible, helping prevent foot, ankle, and leg pain. It begins by first standing and facing the wall, with the arms outstretched and the palms on the wall. Then place one foot behind another keeping the back leg straight, and the forward leg bending at the knee. Make sure both heels are flat on the floor and adjust your stance accordingly. With your hips, lean forward to feel the stretch, you can also adjust the distance from your feet to feel the stretch in various parts of the calf. Make sure to hold the stretch for about 30 seconds and repeat the same process 3 times with each leg. An even easier foot exercise is simply walking on sand. Walking barefoot on sand both strengthens and stretches your feet.
Doing these exercises regularly can help prevent many foot and ankle problems. Other foot exercises can even relieve pain. For example, those affected with plantar fasciitis can simply sit down on a chair, and then place a tennis ball below their affected foot. By rolling the ball under the foot, and increasing or decreasing pressure, pain will be relieved. With any exercise, it is always important to do a small warmup such as walking a few laps around the house to get the blood flowing. If after doing an exercise to relieve pain such as the tennis ball exercise, or are unsure that your execution is correct, be sure to contact a podiatrist for further instruction.
Plantar Fibroma
A plantar fibroma is a knot in the arch of the foot. It can cause pain when repeated pressure is applied by walking barefoot or wearing tight shoes. While plantar fibromas can appear in anyone, men who are middle-aged or older are said to be more susceptible. The main symptom of a plantar fibroma is a firm lump on the arch of the foot. If there is pain, it can be intensified by putting pressure on the nodule. The lump can stay one size or grow larger. You may have one or more fibromas in the feet and there tends to be a high incidence of recurring plantar fibromas. Generally, a plantar fibroma can be treated without surgery. Treatment might include steroid injections to help shrink the lump, orthotics to help redistribute weight away from the nodule, plantar fascia stretching, or physical therapy to help use anti-inflammatory medication on the lump. If a lump grows larger or more painful, a podiatrist can be consulted to confirm the diagnosis. The doctor will palpate the lump and this may cause pain that can be felt all the way to the toes. An X-ray, MRI, or biopsy might be done if further evaluation is necessary. A lump in the arch of the foot might be something other than a plantar fibroma, such as cysts, nerve or fatty tumors, swollen tendons, or an infection in the foot. It is important to see a podiatrist for proper diagnosis and treatment of plantar fibromas.
Definition of a Plantar Fibroma

A plantar fibroma is a benign, firm lump that forms in the arch of the foot within the plantar fascia, a thick band of tissue along the sole. This condition is part of a broader disorder called plantar fibromatosis, where fibrous nodules develop and may grow slowly over time. Causes are not always clear but may include trauma, genetic factors, or connective tissue disorders. Symptoms can involve pain, tenderness, or discomfort while walking or standing. Risk factors include middle age, family history, and certain medical conditions. A podiatrist can evaluate the growth, provide noninvasive treatment, and manage symptoms effectively. If you notice a lump in your foot arch, it is suggested that you consult a podiatrist for early diagnosis and care.
A plantar fibroma may disrupt your daily activities. If you have any concerns, contact one of our podiatrists of Pima Foot and Ankle Surgery. Our doctors can provide the care you need to keep you pain-free and on your feet.
Plantar Fibroma
A plantar fibroma is a fibrous knot in the arch of the foot. It is embedded in the plantar fascia which is a band of tissue that extends from the heel to the toes along the bottom of the foot. There can be multiple plantar fibromas in the feet at the same time. There are no known causes for this condition. If you have a plantar fibroma, there will be a bump in the arch of your foot that cannot be missed. Any associated pain is most often due to a shoe rubbing against the nodule. Non-surgical options, such as steroid injections, physical therapy, and orthotics should be tried first. Surgery is a last resort and is the only thing that will remove a plantar fibroma entirely. Consult with a podiatrist for a proper diagnosis and to determine the treatment regimen that is right for you.
What Causes a Plantar Fibroma?
While there are no specific causes identified, a plantar fibroma can possibly come from genetic predisposition or the formation of scar tissue that forms from healing the tears in the plantar fascia.
What Are the Symptoms of a Plantar Fibroma?
There will be a noticeable lump in the arch of the foot that may or may not cause pain. If pain is felt, it is typically because a shoe is rubbing up against the lump or when walking or standing barefoot.
Treatment and Prevention
A plantar fibroma will not disappear without treatment, but it can get smaller and be a non-issue. If pain persists, a podiatrist examines the foot and when the arch of the foot is pressed, pain can be felt down to the toes. An MRI or biopsy might be performed to help diagnose or evaluate the plantar fibroma. The following non-surgical options are generally enough to reduce the size and pain of these nodules:
- Steroid injections
- Orthotics
- Physical therapy to help apply anti-inflammatory creams on the bump
Surgery is considered if the mass increases in size and the patient continues to feel pain after non-surgical methods are tried.
If you have any questions please feel free to contact our offices located in . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
Understanding Fungal Infections of the Toenail

A fungal toenail infection can begin as a small white or yellow spot and slowly spread deeper into the nail. Over time, the nail may become thick, brittle, discolored, or start to lift from the nail bed. These infections often develop in warm, damp environments and are more common in people who wear tight shoes, walk barefoot in public places, or have a history of athlete’s foot. Poor circulation or a weakened immune system may also increase risk. While the condition is usually not painful early on, it can lead to discomfort or difficulty trimming the nail, if left untreated. More persistent infections often require prescription treatment or professional care. If your toenails are showing signs of thickening, crumbling, or discoloration, it is suggested that you see a podiatrist for proper diagnosis and appropriate treatment.
For more information about treatment, contact one of our podiatrists of Pima Foot and Ankle Surgery. Our doctors can provide the care you need to keep you pain-free and on your feet.
Toenail Fungus Treatment
Toenail fungus is a condition that affects many people and can be especially hard to get rid of. Fortunately, there are several methods to go about treating and avoiding it.
Antifungals & Deterrence
Oral antifungal medicine has been shown to be effective in many cases. It is important to consult with a podiatrist to determine the proper regiment for you, or potentially explore other options.
Applying foot powder on the feet and shoes helps keep the feet free of moisture and sweat.
Sandals or open toed shoes – Wearing these will allow air movement and help keep feet dry. They also expose your feet to light, which fungus cannot tolerate. Socks with moisture wicking material also help as well.
If you have any questions please feel free to contact our offices located in . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
Treating Toenail Fungus
Fungal infection of the toenail, or onychomycosis, typically appears as a gradual change in a toenail’s texture and color that involves brittleness and darkening. The fungal infection itself occurs beneath the surface of the nail. Aside from discoloration, other symptoms include the collection of debris beneath the nail plate, white marks on the nail plate, and a foul odor emanating from the nail. If ignored, the infection can spread into other nails and the skin; in severe cases, it can hinder one’s ability to work or walk.
The toenails are particularly vulnerable to contracting infection in moist environments where people are likely to be walking barefoot, such as around swimming pools, public showers, and locker rooms. Fungal infection may also be more likely to occur in nail beds that have been injured, and sufferers of chronic diseases such as diabetes, circulatory problems, or immunodeficiency conditions are particularly prone to developing fungal nails.
Fungal nails can be primarily prevented by practicing proper hygiene and regularly examining the feet and toes. Carefully washing the feet with soap and water and thoroughly drying the feet afterwards are essential. Other tips include wearing shower shoes in public areas, changing shoes and socks daily, keeping toenails clipped at a short length, wearing breathable shoes that fit properly, wearing moisture-wicking socks, and disinfecting home pedicure tools and instruments used to cut nails.
Fungal nail treatment may vary between patients and the severity of the condition. Your podiatrist may suggest a daily routine of cleansing that spans over a period of time to ease mild infections. Over-the-counter or prescription antifungal agents may also be prescribed, including topical and/or oral medications. Debridement, or the removal of diseased nail matter and debris, may also be performed. In more severe cases, surgical treatment may be needed. In some instances, the temporary removal of the fungal nail allows for the direct application of a topical antifungal to the nail bed. In other cases, a chronically painful fungal nail that has not responded to other treatments may be permanently removed; this allows the infection to be cured and avoids the growth of a deformed nail.
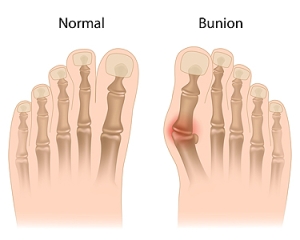
Understanding Bunions and Their Risk Factors
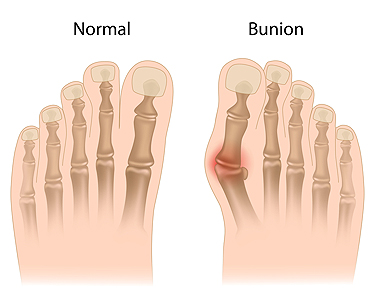
A bunion is a bony bump that forms at the base of the big toe, caused when the tip of the toe lean toward the others. This misalignment is often the result of inherited foot structure, improper footwear, or conditions like arthritis. Risk factors include family history, flat feet, and wearing tight or pointed shoes. Prevention includes wearing shoes with wide a toe box, using supportive shoe inserts, and avoiding high heels. A podiatrist can assess foot structure, recommend custom orthotics, and provide treatment to relieve pain or suggest surgical correction, when necessary. If you are experiencing discomfort near your big toe or notice a visible bump, it is suggested that you schedule an appointment with a podiatrist who can offer relief and treatment tips.
If you are suffering from bunion pain, contact one of our podiatrists of Pima Foot and Ankle Surgery. Our doctors can provide the care you need to keep you pain-free and on your feet.
What Is a Bunion?
Bunions are painful bony bumps that usually develop on the inside of the foot at the joint of the big toe. As the deformity increases over time, it may become painful to walk and wear shoes. Women are more likely to exacerbate existing bunions since they often wear tight, narrow shoes that shift their toes together. Bunion pain can be relieved by wearing wider shoes with enough room for the toes.
Causes
- Genetics – some people inherit feet that are more prone to bunion development
- Inflammatory Conditions - rheumatoid arthritis and polio may cause bunion development
Symptoms
- Redness and inflammation
- Pain and tenderness
- Callus or corns on the bump
- Restricted motion in the big toe
In order to diagnose your bunion, your podiatrist may ask about your medical history, symptoms, and general health. Your doctor might also order an x-ray to take a closer look at your feet. Nonsurgical treatment options include orthotics, padding, icing, changes in footwear, and medication. If nonsurgical treatments don’t alleviate your bunion pain, surgery may be necessary.
If you have any questions, please feel free to contact our offices located in . We offer the newest diagnostic and treatment technologies for all your foot care needs.
What Are Bunions?
Bunions are large bony bumps at the base of the big toe. Medically known as hallux valgus, a bunion is a misalignment of the metatarsophalangeal joint, or big toe joint. The misalignment will generally worsen with time if left untreated.
The exact cause of bunions is unknown, with genetics seen as a potential cause. High heels and poorly-fitted footwear, rheumatoid arthritis, and heredity all seem to be potential factors behind the exacerbation of bunions. Women have been found to be more likely to develop bunions in comparison to men.
Bunions do not always produce symptoms. The best way to tell is if the big toe is pushing up against the next toe and there is a large protrusion at the base of the big toe. You may or may not feel pain. Redness, swelling, and restricted movement of the big toe may be present as well.
Podiatrists use a variety of methods to diagnose bunions. If there are symptoms present, podiatrists will first consider that it is a bunion. If not, a physical examination will be conducted to check function of the big toe. Finally, an X-ray may be taken to view the extent of the bunion and confirm it is a bunion.
Typically, nonsurgical methods are used to treat bunions, unless the bunion has become too misaligned. Orthotics, icing and resting the foot, roomier and better fitted shoes, taping the foot, and pain medication are usually utilized first. If the bunion doesn’t go away or causes extreme pain, surgery may be required. Surgeons will either remove part of the swollen tissue or bone to straighten the toe out.
If you have a bunion, it is recommended to see a podiatrist. The longer it is left untreated, the worse it may get. Podiatrists can properly diagnose and treat a bunion before it gets worse.
Recognizing Rheumatoid Arthritis in the Feet

Rheumatoid arthritis in the feet is an autoimmune condition where the immune system attacks the joints, leading to inflammation, pain, and stiffness. It often begins in the small joints of the toes and feet, causing swelling, redness, and difficulty walking. Over time, it may lead to joint deformities and loss of function. The exact cause is unknown, but genetics and environmental triggers may play a role. Risk factors include family history, smoking, and age. A podiatrist can help by evaluating joint function, reducing pain through custom orthotics, and recommending strategies to maintain mobility. If you notice persistent foot pain or swelling, it is strongly suggested that you consult a podiatrist who can offer effective relief and management strategies.
Because RA affects more than just your joints, including the joints in your feet and ankles, it is important to seek early diagnosis from your podiatrist if you feel like the pain in your feet might be caused by RA. For more information, contact one of our podiatrists of Pima Foot and Ankle Surgery. Our doctors will assist you with all of your podiatric concerns.
What Is Rheumatoid Arthritis?
Rheumatoid Arthritis (RA) is an autoimmune disorder in which the body’s own immune system attacks the membranes surrounding the joints. Inflammation of the lining and eventually the destruction of the joint’s cartilage and bone occur, causing severe pain and immobility.
Rheumatoid Arthritis of the Feet
Although RA usually attacks multiple bones and joints throughout the entire body, almost 90 percent of cases result in pain in the foot or ankle area.
Symptoms
- Swelling and pain in the feet
- Stiffness in the feet
- Pain on the ball or sole of feet
- Joint shift and deformation
Diagnosis
Quick diagnosis of RA in the feet is important so that the podiatrist can treat the area effectively. Your doctor will ask you about your medical history, occupation, and lifestyle to determine the origin of the condition. Rheumatoid Factor tests help to determine if someone is affected by the disease.
If you have any questions please feel free to contact our offices located in . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.