Causes and Symptoms of Heel Fissures

Heel fissures are cracks in the skin over your heels that can range from minor discomfort to serious health concerns. Symptoms include can mild discoloration, thickening of the skin, visible splitting of the skin, and bleeding. Without treatment, heel fissures can worsen, leading to open wounds, pain, and even deep ulcers susceptible to infections like cellulitis. Dry skin on the heels is a primary cause of fissures, worsened by conditions such as diabetes, eczema, and fungal infections. Due to damaged foot nerves and decreased moisture, diabetic patients are particularly at risk for heel fissures that progress into non-healing ulcers. To manage symptoms of heel fissures, regular moisturizing is recommended, in addition to exfoliation with alpha hydroxy acids or urea-based creams. If the heel fissures continue to worsen, seeking medical attention from a podiatrist is suggested. This foot doctor can provide specialized debridement to remove thickened skin and prescribe medication to combat infections. If dry skin on your feet is causing problems like heel fissures, it is suggested that you schedule an appointment with a podiatrist.
Cracked heels are unsightly and can cause further damage to your shoes and feet. If you have any concerns, contact one of our podiatrists from Pima Foot and Ankle Surgery. Our doctors can provide the care you need to keep you pain-free and on your feet.
Cracked Heels
Cracked heels appear unappealing and can make it harder for you walk around in sandals. Aside from looking unpleasant, cracked heels can also tear stockings, socks, and wear out your shoes. There are several methods to help restore a cracked heel and prevent further damage.
How Do You Get Them?
Dry skin is the number one culprit in creating cracked heels. Many athletes, walkers, joggers, and even swimmers suffer from cracked heels. Age and skin oil production play a role to getting cracked heels as well.
Promote Healing
Over the counter medicines can help, especially for those that need instant relief or who suffer from chronic dry feet.
Wear Socks – Wearing socks with medicated creams helps lock in moisture.
Moisturizers – Applying both day and night will help alleviate dryness which causes cracking.
Pumice Stones – These exfoliate and remove dead skin, which allows for smoother moisturizer application and better absorption into the skin.
Change in Diet
Eating healthy with a well-balanced diet will give the skin a fresh and radiant look. Your body responds to the kinds of food you ingest. Omega-3 fatty acids and zinc supplements can also revitalize skin tissue.
Most importantly, seek professional help if unsure how to proceed in treating cracked heels. A podiatrist will help you with any questions or information needed.
If you have any questions, please feel free to contact our offices located in . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Solutions for Cracked Heels
Cracked heels can make life very frustrating and embarrassing when displaying the bare feet. Aside from being unpleasing to the eye, they can also tear stockings and socks and wear out shoes at a faster rate. When severe, cracked heels may cause pain or infection.
Cracked heels are a problem for those who are athletic, those who may walk a lot, and those who have especially dry skin. Those who use medication that dry the skin, those who swim often, wearing certain types of shoes, and those who are diabetic may have trouble with cracked heels. Seniors whose skin produces less oil may also have trouble with cracked feet. There is no one way to develop cracked feet, and there is no cure.
Today, the market consists of numerous products that have a variety of ingredients to promote healing. Some of these are over-the-counter. Others are prescribed by a doctor, especially for those who have chronic dry feet and heels.
Some doctors recommend wearing socks at night for those with rough skin. This helps further healing, and helps creams stay on longer and better absorb into the skin.
One way to alleviate dryness that causes cracked heels is by using moisturizers both day and night. Another way is to make sure the skin is clean and dry at all times. Using a pumice stone to buff away dead skin before putting on moisturizer can also help. Cracked heels will not respond to the cream unless the outer layer of skin is first removed through exfoliation. After exfoliation, lotion or ointment will be absorbed by the skin more easily.
Foods that produce healing and balance can also help the skin from within. Everything that is put into the body can either help it or hurt it. Taking supplements of omega-3 fatty acids and zinc can also be very beneficial.
Nevertheless, not all products are guaranteed to help treat cracked feet. Seeing a professional is best if other treatments options were unsuccessful. A podiatrist should be able to give the best advice to help with this problem.
How Athlete’s Can Safeguard Against Plantar Fasciitis
Athletes employ various tactics to shield themselves from the discomfort of plantar fasciitis, a common ailment among active individuals. Proper footwear selection plays a pivotal role, with athletes opting for supportive shoes that offer ample cushioning and stability. Additionally, incorporating stretching and strengthening exercises into their routine helps maintain flexibility and strength in the muscles and ligaments of the feet and lower legs, reducing the risk of strain and injury. Gradual progression in training intensity and duration also proves beneficial, allowing the body to adapt gradually to increased demands and minimizing the likelihood of overuse injuries like plantar fasciitis. Podiatrists may prescribe orthotic inserts or arch supports that can provide additional support and alignment for the feet. If you have heel pain, it is suggested that you consult with this type of doctor who can treat plantar fasciitis, and provide effective preventive solutions.
Plantar fasciitis can be very painful and inconvenient. If you are experiencing heel pain or symptoms of plantar fasciitis, contact one of our podiatrists from Pima Foot and Ankle Surgery. Our doctors can provide the care you need to keep you pain-free and on your feet.
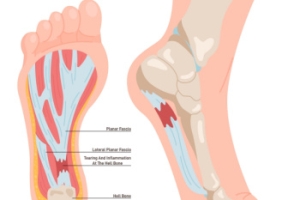
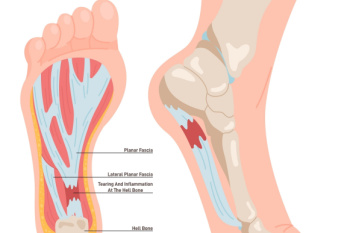
What Is Plantar Fasciitis?
Plantar fasciitis is the inflammation of the thick band of tissue that runs along the bottom of your foot, known as the plantar fascia, and causes mild to severe heel pain.
What Causes Plantar Fasciitis?
- Excessive running
- Non-supportive shoes
- Overpronation
- Repeated stretching and tearing of the plantar fascia
How Can It Be Treated?
- Conservative measures – anti-inflammatories, ice packs, stretching exercises, physical therapy, orthotic devices
- Shockwave therapy – sound waves are sent to the affected area to facilitate healing and are usually used for chronic cases of plantar fasciitis
- Surgery – usually only used as a last resort when all else fails. The plantar fascia can be surgically detached from the heel
While very treatable, plantar fasciitis is definitely not something that should be ignored. Especially in severe cases, speaking to your doctor right away is highly recommended to avoid complications and severe heel pain. Your podiatrist can work with you to provide the appropriate treatment options tailored to your condition.
If you have any questions please feel free to contact our offices located in . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Plantar Fasciitis
The plantar fascia is a connective tissue in the heel that stretches across the bottom length of your foot. Plantar fasciitis occurs when the connective tissue becomes inflamed, causing heel pain and discomfort during physical activity. Although the condition is completely treatable, traditional methods can take up to a year to start becoming effective.
Plantar fasciitis is caused by a number of everyday activities, so understanding the condition is important for managing and treating it. One of the most common causes of plantar fasciitis is excessive running, especially with improper fitting or non-supportive shoes. Too much exercise can lead to the plantar fascia being overworked and overstretched, which can cause tears in the tissue. Along with improper fitting shoes, pronation, the rolling of the feet inward, is a common cause of plantar fasciitis. If not treated properly, the plantar fascia becomes overstretched and starts to tear, causing inflammation.
Despite the common causes of plantar fasciitis, there are many different treatment options. For less severe cases, conservative home remedies include taking anti-inflammatory drugs to alleviate pain, applying ice packs to the bottom of your foot and heel, slowly stretching and exercising your feet to re-strengthen the tissue, and using orthotic devices are all ways to help manage your plantar fasciitis.
For more severe cases, shockwave therapy has become a common solution for plantar fasciitis. Shockwave therapy can effectively break up the tissue on the bottom of your foot which facilitates healing and regeneration. This fights the chronic pain caused by plantar fasciitis. Even if this doesn’t work, surgery is always a final option. Surgery on the tissue itself can be done to permanently correct the issue and stop the inflammation and pain in your heels.
No matter what the case may be, consulting your podiatrist is the first and best step to recovery. Even the slightest amount of heel pain could be the first stage of plantar fasciitis. Untreated symptoms can lead to the tearing and overstretching of tissue. Because the tearing of tissue can be compounded if it remains ignored, it can evolve into a severe case. The solution is early detection and early treatment. Talk to your podiatrist about the possibilities of plantar fasciitis if you’re experiencing heel pain.
Peripheral Artery Disease and Diabetes
 Peripheral artery disease, or PAD, is a condition where the arteries that supply blood to the legs and feet become narrowed due to plaque buildup. Diabetes significantly increases the risk of developing this condition. High blood sugar levels contribute to the accumulation of fatty deposits in the blood vessels, which can harden and reduce blood flow. This process, known as atherosclerosis, is more common in diabetes patients due to the chronic high glucose levels that damage the blood vessel walls. Symptoms of PAD include pain, cramping, or heaviness in the legs and feet during activities like walking. Complications like ulcers, which often appear on the feet, can lead to serious infections. Regular check-ups with a podiatrist, or foot doctor, are important to prevent any issues and manage foot and lower leg health. If you have symptoms of peripheral artery disease, it is suggested that you make an appointment with a podiatrist today.
Peripheral artery disease, or PAD, is a condition where the arteries that supply blood to the legs and feet become narrowed due to plaque buildup. Diabetes significantly increases the risk of developing this condition. High blood sugar levels contribute to the accumulation of fatty deposits in the blood vessels, which can harden and reduce blood flow. This process, known as atherosclerosis, is more common in diabetes patients due to the chronic high glucose levels that damage the blood vessel walls. Symptoms of PAD include pain, cramping, or heaviness in the legs and feet during activities like walking. Complications like ulcers, which often appear on the feet, can lead to serious infections. Regular check-ups with a podiatrist, or foot doctor, are important to prevent any issues and manage foot and lower leg health. If you have symptoms of peripheral artery disease, it is suggested that you make an appointment with a podiatrist today.
Peripheral artery disease can pose a serious risk to your health. It can increase the risk of stroke and heart attack. If you have symptoms of peripheral artery disease, consult with one of our podiatrists from Pima Foot and Ankle Surgery. Our doctors will assess your condition and provide you with quality foot and ankle treatment.
Peripheral artery disease (PAD) is when arteries are constricted due to plaque (fatty deposits) build-up. This results in less blood flow to the legs and other extremities. The main cause of PAD is atherosclerosis, in which plaque builds up in the arteries.
Symptoms
Symptoms of PAD include:
- Claudication (leg pain from walking)
- Numbness in legs
- Decrease in growth of leg hair and toenails
- Paleness of the skin
- Erectile dysfunction
- Sores and wounds on legs and feet that won’t heal
- Coldness in one leg
It is important to note that a majority of individuals never show any symptoms of PAD.
Diagnosis
While PAD occurs in the legs and arteries, Podiatrists can diagnose PAD. Podiatrists utilize a test called an ankle-brachial index (ABI). An ABI test compares blood pressure in your arm to you ankle to see if any abnormality occurs. Ultrasound and imaging devices may also be used.
Treatment
Fortunately, lifestyle changes such as maintaining a healthy diet, exercising, managing cholesterol and blood sugar levels, and quitting smoking, can all treat PAD. Medications that prevent clots from occurring can be prescribed. Finally, in some cases, surgery may be recommended.
If you have any questions, please feel free to contact our offices located in . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Peripheral Artery Disease
Peripheral artery disease (PAD), or peripheral arterial disease, is a circulatory problem in which there is a reduction of blood flow to the limbs due to narrowed arteries. When peripheral artery disease develops, the extremities do not receive enough blood flow; this may cause symptoms to develop such as claudication, or leg pain when walking. The legs are the most common site of peripheral artery disease.
Claudication, or leg pain when walking, is one of several symptoms that can develop due to peripheral artery disease. Other symptoms caused by the disease include painful cramping in the hips, thighs, or calves after certain activities; leg numbness or weakness; coldness in the lower leg or foot; sores on the lower extremities that do not heal; hair loss on the lower extremities; and a missing or weak pulse in the lower extremities. In more severe cases, pain may even occur when the body is at rest or when lying down.
Peripheral artery disease is typically caused by atherosclerosis, a condition in which fatty deposits build up in the arterial walls and reduce blood flow. Smoking, diabetes, obesity, high blood pressure, and high cholesterol are some of the risk factors for peripheral artery disease.
If you are experiencing pain, numbness, or other symptoms in the lower extremities, see your healthcare professional immediately. Diagnosed peripheral artery disease can be treated with various medications, angioplasty and surgery, exercise programs, or alternative medicine. It is important to consult a healthcare professional to determine the best treatment for you.
Treating Ankle Sprains
 Ankle sprains are injuries that occur when the ligaments that support the ankle stretch beyond their limits or tear. These injuries are often caused by twisting the ankle during physical activities, such as sports or even walking on uneven surfaces. Treatment for ankle sprains ranges from conservative to more intensive approaches, depending on the severity of the sprain. Initial treatment for mild sprains typically includes rest and elevation to reduce swelling and pain. More severe sprains may require immobilization with a brace or cast to allow the ligaments to heal properly. Certain stretches may be recommended to restore ankle strength, flexibility, and balance, and prevent future sprains. In cases where the ligament damage is extensive and stability is compromised, surgical intervention may be considered to repair the ligaments. If you have sprained your ankle, it is suggested that you promptly schedule an appointment with a podiatrist to get the right treatment.
Ankle sprains are injuries that occur when the ligaments that support the ankle stretch beyond their limits or tear. These injuries are often caused by twisting the ankle during physical activities, such as sports or even walking on uneven surfaces. Treatment for ankle sprains ranges from conservative to more intensive approaches, depending on the severity of the sprain. Initial treatment for mild sprains typically includes rest and elevation to reduce swelling and pain. More severe sprains may require immobilization with a brace or cast to allow the ligaments to heal properly. Certain stretches may be recommended to restore ankle strength, flexibility, and balance, and prevent future sprains. In cases where the ligament damage is extensive and stability is compromised, surgical intervention may be considered to repair the ligaments. If you have sprained your ankle, it is suggested that you promptly schedule an appointment with a podiatrist to get the right treatment.
Ankle sprains are common but need immediate attention. If you need your feet checked, contact one of our podiatrists from Pima Foot and Ankle Surgery. Our doctors can provide the care you need to keep you pain-free and on your feet.
How Does an Ankle Sprain Occur?
Ankle sprains take place when the ligaments in your ankle are torn or stretched beyond their limits. There are multiple ways that the ankle can become injured, including twisting or rolling over onto your ankle, putting undue stress on it, or causing trauma to the ankle itself.
What Are the Symptoms?
- Mild to moderate bruising
- Limited mobility
- Swelling
- Discoloration of the skin (depending on severity)
Preventing a Sprain
- Wearing appropriate shoes for the occasion
- Stretching before exercises and sports
- Knowing your limits
Treatment of a Sprain
Treatment of a sprain depends on the severity. Many times, people are told to rest and remain off their feet completely, while others are given an air cast. If the sprain is very severe, surgery may be required.
If you have suffered an ankle sprain previously, you may want to consider additional support such as a brace and regular exercises to strengthen the ankle.
If you have any questions please feel free to contact our offices located in . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Ankle Sprains
Although ankle sprains may not be as serious as a broken ankle, they should be given immediate attention and care. An ankle sprain can lead to a significant amount of pain, as well as limited mobility. They are often characterized by the swelling and discoloration of the skin. This occurs when the ligaments are stretched beyond their limits.
The simple act of walking can sometimes cause a sprain, which makes ankle sprains a very common injury that can happen to anyone. They occur when the ankle twists in an awkward way or rolls over itself, causing a pop or snap in the tendons around the ankle. Some people are more at risk than others. These include athletes who continually push their bodies to the limits and also people who have previously suffered accidents to the feet, ankles, or lower legs.
Most of the time, an ankle sprain is not severe enough for hospital attention. There are many at-home treatment options available, including propping the leg up above your head to reduce blood flow and inflammation, applying ice packs to the affected area as needed, taking over-the-counter pain relievers and anti-inflammatory medication, using an ACE bandage to wrap and support the injured ankle, and most importantly, remaining off your feet until the ankle has fully healed.
Despite this, an ankle sprain can turn into a severe injury that might require hospitalization. If the ankle ligaments or muscles are damaged from a tear or rip, that is one sign that the sprain is severe enough for hospital attention and possibly for surgery. Even after the surgery, the recovery process can be long. You may need to have rehabilitation sessions administered by your podiatrist to get your ankle back to full health.
The severity of your sprain might become apparent if you are unable to stand or walk, consistent pain occurs over a prolonged period of time, swelling is much more severe than initially present, or if you start to experience tingling or numbness. These signs may indicate that your ankle sprain might actually be a broken ankle, an injury that requires immediate medical attention.
Although they are not completely avoidable, ankle sprains can be curbed with some preventative treatment measures. These include wearing appropriate-fitting shoes that not only provide a comfortable fit, but also ankle support. It is also recommended to stretch before doing any kind of physical activity, as this will help lower your body’s chance for an injury.
What Is Athlete’s Foot?
 Athlete's foot is a fungal infection that affects the skin of the feet. It's caused by various types of fungi that thrive in warm, moist environments. Athlete’s foot is commonly contracted in places such as locker rooms, swimming pools, and communal showers. When the feet are exposed to these fungi, they can easily penetrate the skin, leading to the development of athlete's foot. Factors such as wearing tight or poorly ventilated shoes, sweating excessively, or having a weakened immune system can increase the risk of developing athlete’s foot. Athlete’s foot is highly contagious and can spread through direct contact with infected skin or by sharing contaminated items like towels or shoes. Symptoms of athlete's foot include itching, redness, and peeling of the skin between the toes or on the soles of the feet. Podiatrists, or foot doctors, are well-equipped to diagnose and treat athlete's foot. They may offer treatments, such as antifungal medications and topical treatments to help patients find relief. If you suspect athlete’s foot, it is suggested that you consult a podiatrist for prompt treatment.
Athlete's foot is a fungal infection that affects the skin of the feet. It's caused by various types of fungi that thrive in warm, moist environments. Athlete’s foot is commonly contracted in places such as locker rooms, swimming pools, and communal showers. When the feet are exposed to these fungi, they can easily penetrate the skin, leading to the development of athlete's foot. Factors such as wearing tight or poorly ventilated shoes, sweating excessively, or having a weakened immune system can increase the risk of developing athlete’s foot. Athlete’s foot is highly contagious and can spread through direct contact with infected skin or by sharing contaminated items like towels or shoes. Symptoms of athlete's foot include itching, redness, and peeling of the skin between the toes or on the soles of the feet. Podiatrists, or foot doctors, are well-equipped to diagnose and treat athlete's foot. They may offer treatments, such as antifungal medications and topical treatments to help patients find relief. If you suspect athlete’s foot, it is suggested that you consult a podiatrist for prompt treatment.
Athlete’s foot is an inconvenient condition that can be easily reduced with the proper treatment. If you have any concerns about your feet and ankles, contact one of our podiatrists from Pima Foot and Ankle Surgery. Our doctors will treat your foot and ankle needs.
Athlete’s Foot: The Sole Story
Athlete's foot, also known as tinea pedis, can be an extremely contagious foot infection. It is commonly contracted in public changing areas and bathrooms, dormitory style living quarters, around locker rooms and public swimming pools, or anywhere your feet often come into contact with other people.
Solutions to Combat Athlete’s Foot
- Hydrate your feet by using lotion
- Exfoliate
- Buff off nails
- Use of anti-fungal products
- Examine your feet and visit your doctor if any suspicious blisters or cuts develop
Athlete’s foot can cause many irritating symptoms such as dry and flaking skin, itching, and redness. Some more severe symptoms can include bleeding and cracked skin, intense itching and burning, and even pain when walking. In the worst cases, Athlete’s foot can cause blistering as well. Speak to your podiatrist for a better understanding of the different causes of Athlete’s foot, as well as help in determining which treatment options are best for you.
If you have any questions please feel free to contact our offices located in . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.